Gastrointestinal Conditions and the Endocannabinoid System
By Diana Hahn and Stacey Marie Kerr MD
Recent studies have found that the endocannabinoid system (ECS) plays a significant role in the functioning and health of the gastrointestinal system. These findings support the historical use of cannabis to treat digestive disorders dating back centuries. [1]
The Endocannabinoid System and Digestion
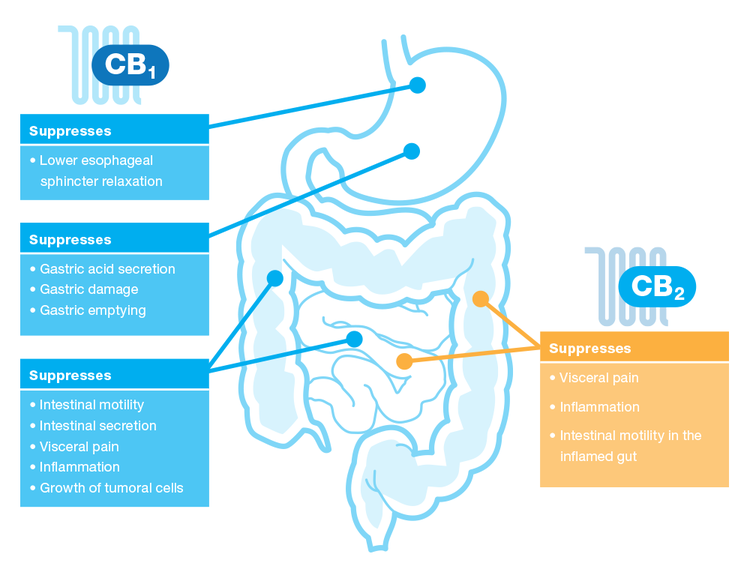
All major components of the ECS, including cannabinoid receptors, endocannabinoids, and both synthesizing and degrading enzymes are present throughout the GI tract. Interplay between the ECS and the enteric nervous system (nervous system of the GI tract) contribute to the regulation of food intake, nausea, vomiting, gastric secretion, gastroprotection, GI motility, visceral sensation, intestinal inflammation, and cell proliferation in the gut. [1]
Cannabis as a Treatment for IBS and IBD
Studies show cannabis can be effective in treating inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, as well as irritable bowel syndrome (IBS).
Inflammatory Bowel Disease
Cannabis has been observed to be beneficial to patients with IBD. While the exact mechanisms of how cannabis helps these conditions are not clear, the known anti-inflammatory, analgesic, and immunomodulatory properties of cannabinoids combined with the ECS’ significant presence in the GI tract may provide a foundation for further research.
Inflammatory bowel disease is a significant life-changing diagnosis that causes severe diarrhea, pain, fatigue and weight loss. There is a genetic predisposition for IBD, and it can be life-threatening. IBD is defined as chronic inflammation in the digestive tract, and includes conditions such as Crohn’s disease (CD) and ulcerative colitis (UC).
Both CD and UC are caused by an inappropriate immune response to normal intestinal flora. Increased permeability of membranes in the GI tract leads to the activation of the immune system, triggering a “cascade effect” of immune response and consequently inflammation. [2] CB1 and CB2 receptors are present through much of this inflammation cascade pathway, and may be involved in both peripheral (gut) and central (brain and central nervous system) actions. [3]
Conventional treatments for IBD include many pharmaceuticals to control symptoms including steroids, immunomodulators, aminosalicylates, and antibiotics. Surgery may be necessary for UC. [4] These treatment options often come with significant risks and adverse effects. Combined with limited efficacy, severity of disease, and there being no known cure for IBD, research into new treatment options as well as a greater understanding of the disease would greatly benefit patients living with IBD.
Medical cannabis is a promising new treatment option for IBD. Cannabinoids have been shown to be anti-inflammatory, mainly through CB2 receptors. Cannabinoids shift the balance of pro-inflammatory cytokines to anti-inflammatory cytokines, as well as down-regulating the production of pro-inflammatory cytokines. [4] So far, we have seen that THC and CBD taken together have a better effect than either cannabinoid alone. [4]
A study done with Crohn’s disease patients provides promising information, suggesting that cannabis is worth considering for patients who do not respond to conventional therapies.
| Study Description | |
|---|---|
| Size | 21 patients, mean age 40, 13 men and 8 women |
| Crohn’s Disease Activity Index (CDAI) | All patients started between 200-450 |
| Patient Screening | All participants were unresponsive to steroids, immuno-modulators, or anti-tumor necrosis factor-a treatments, and had no experience with cannabis. |
| Study Design | Test group received cannabis twice a day, in the form of cannabis cigarettes made with 23% THC, <.5% CBD controlled flowers. Placebo group received cannabis cigarettes with THC removed twice a day. Disease activity was monitored for 8 weeks of treatment and 2 weeks thereafter. |
| Results | ||
|---|---|---|
| Cannabis | Placebo | |
| Complete Remission (CDAI < 150) | 45% achieved | 10% achieved |
| Clinical Response (Decrease in CDAI >100) | 90% achieved | 40% achieved |
| Average reduction in CDAI | 177 | 66 |
In addition, 3 patients were able to stop using steroids and 2 patients were able to stop using opioids in the cannabis group. Interestingly, reporting on adverse effects including sleepiness, nausea, confusion, dizziness, concentration and memory loss were the same for the cannabis and placebo groups. Positive side effects, including pain relief, appetite, and satisfaction were significantly higher for the cannabis treatment group. No serious adverse effects were reported. [3]
CBD-rich cannabis extracts (approximately 64% CBD, 3% THC) have been shown to be effective at reducing GI tract inflammation and hypermotility (diarrhea) in animal models. The same study also showed that although CBD can reduce diarrhea, it does not cause constipation in normal animals. Of note, pure CBD was not as effective as a botanical extract that was rich in CBD, but contained THC as well as other cannabinoids. While these results have yet to be reproduced in humans, they suggest that CBD-dominant strains and extracts may be effective at treating IBD. Experimenting with CBD may be worth trying for IBD patients who cannot tolerate the psychoactive effects of THC.
Irritable Bowel Syndrome
IBS is thought to be a combination of abnormal GI tract motility and a disruption of the communication between the brain and the GI tract. Symptoms include gastrointestinal pain, cramping, bloating, and varying degrees of constipation or diarrhea. [6] IBS affects as many as 20% of the population in western countries, and accounts for 50% of referrals to GI specialists. [7] Despite the prevalence of this condition, little is known about its origin, and conventional treatment options offer limited relief with the possibility of serious side effects that in some cases include fatality. [6]
Recently, the ECS has been recognized as a crucial site of the pathophysiology of IBS. [7] Research suggests that abnormalities in the quantity and breakdown of endocannabinoids (2-AG and anandamide) and endocannabinoid-like fatty acids may be related to whether a patient has diarrhea dominant vs. constipation dominant IBS. [7] Correlations between centralized pain sensitivity and incidence of IBS, migraines, and fibromyalgia also point to the possibility of ECS deficiency being one of the root causes of all three conditions. [6]
Although there is limited clinical research on treating IBS specifically with cannabis, anecdotal evidence reports that cannabis is an effective treatment, and is most often consumed via inhalation. For IBS, pure THC is not effective in treating symptoms, suggesting that whole plant medicines or medicines combining THC with CBD are preferable. [7] While smoking is not recommended by the Department of Health, it does provide faster relief with greater titration control than orally ingested medicines. Vaporizing may present an alternative to smoking that provides relief quickly while limiting the adverse effects of smoking.
Sources:
Izzo AA and Sharkey KA. Cannabinoids and the Gut: New Developments and Emerging Concepts. Pharmacology and Therapeutics. 126 (2010) 21-38.
Wright KL, Duncan M, and Sharkey KA. Cannabinoid CB2 Receptors in the Gastrointestinal Tract: A Regulatory System in States of Inflammation. British Journal of Pharmacology (2008) 153, 263–270
Schicho R and Storr M. Cannabis Finds its Way into Treatment of Crohn’s Disease. Pharmacology 2014; 93:1–3 DOI: 10.1159/000356512
Naftali T, et al. Cannabis Induces a Clinical Response in Patients with Crohn’s Disease: A Prospective Placebo-Controlled Study. Clinical Gastroenterology and Hepatology 2013; 11: 1276-1280.
Pagano E, Capasso R, et al. An Orally Active Cannabis Extract with High Content in Cannabidiol Attenuates Chemically-Induced Intestinal Inflamation and Hypermotility in the Mouse. Frontiers in Pharmacology. 04 October 2016. doi: 10.3389f/phar.2016.00341.
Russo E. Clinical Endocannabinoid Deficiency (CECD): Can This Concept Explain Therapeutic Benefits of Cannabis in Migraine, Fibromyalgia, Irritable Bowel Syndrome and Other Treatment-Resistant Conditions? NeuroendocrinologyLetters. Nos.1/2, Feb-Apr Vol.25, 2004
Fichna J, Wood JT, Papanastasiou M, Vadivel SK, Oprocha P, et al. (2013) Endocannabinoid and Cannabinoid-Like Fatty Acid Amide Levels Correlate with Pain-Related Symptoms in Patients with IBS-D and IBS-C: A Pilot Study. PLoS ONE 8(12): e85073. doi:10.1371/journal.pone.0085073

![[3]](https://images.squarespace-cdn.com/content/v1/5956fd9ae110eba6434be862/1500334871120-GLY3FL4SNL281PJ3ZLUE/image-asset.png)